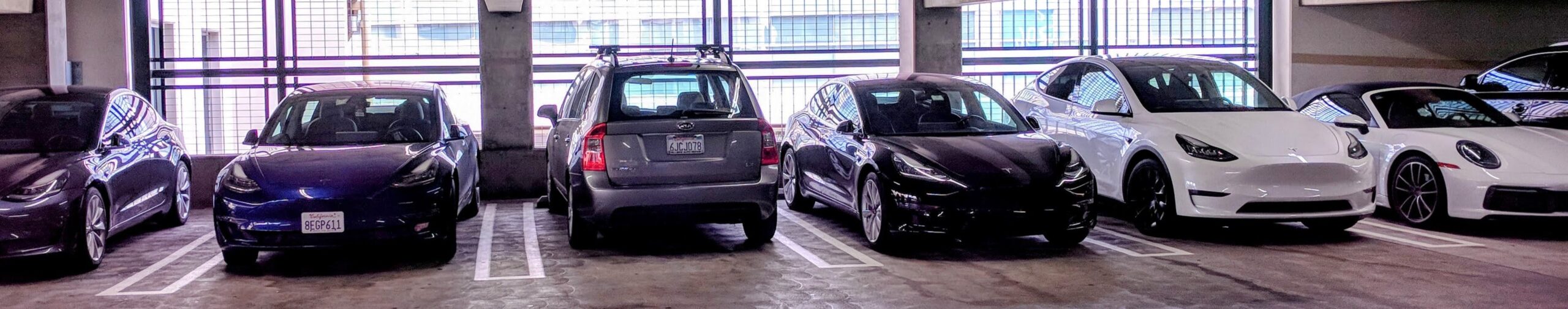
One of these things is not like the other ones...
In part 1, I laid out my perceived options for getting out of night shifts. Here, in part 2, I'll let you know what actually happened at that time.
Dear reader, let's travel back in time several years. Even accounting for the reversal of aging we've just agreed to entertain, I'm older, crankier, and more cantankerous than my younger self. The nights are getting to me more than they used to.
Let's briefly review the options I'd laid out in the companion post as an emergency physician feeling his age:
- Cut my clinical load to the bare minimum, so that while I'm still working nights, I'm working fewer than I otherwise would.
- Change jobs to a place that lets me opt out of nights and receive less pay for that privilege.
- Become a per diem physician and work exclusively days if possible.
- Urgent care.
- Pursue non-clinical work.
- Pull the FI ripcord and parachute into early retirement.
What actually happened at the time? After creating the menu above, I ended up - wait for it - ordering off the menu!
I spent several afternoons emailing and calling friends and acquaintances, reaching out to fellow bloggers and former classmates, all to figure out how they dealt with this problem.
Through membership in a professional network of independent emergency medicine groups, I also connected with the directors of ER groups that had contended with just this problem. How had they equitably balanced the whining of the group elders with fairness to the younger members of the group?
It turned out that the latter tactic was the most helpful strategy. The directors enumerated a number of different strategies.
Death with Dignity
Most groups had an age (usually 60 or over) after which older docs worked either reduced or no nightshifts. Whether this "death with dignity" clause became a source of resentment tended to reflect on the age composition of the group in question.
If a group had a balanced number of younger, mid-career and older physicians, then it was generally accepted as fair. In a large group with mostly younger and mid-career physicians, the small number of older docs exiting the pool of nights was not deemed a burden since their shifts were redistributed among a large group, and the individual impact was minor.
Where it failed was in a bimodal distribution of young and older docs, or in groups where older docs significantly outnumbered younger ones. The group elders felt they'd put in their dues and it was only fair that their contribution to the speciality warranted a glide path without nightshifts.
The younger members did not dispute the contribution , but they did resent being asked to shoulder the burden of the nights. Why should the younger docs meet what they might deem to be an unreasonable expectation, especially when they had no guarantee that they'd get to enjoy a similar entitlement? Such inequalities were felt more acutely in groups where older docs had achieved partner or equity status, while young docs were still working toward that status.
At the risk of beating a dead horse, not all late shifts were considered "nightshifts" by all groups. An elder doc who no longer got assigned "nights" might still be expected to routinely work shifts ending at 2am or later in some of the groups.
Nocturnists
Some groups hired nocturnists and paid them handsomely to take disproportionate night shifts. This worked really well if you lucked out and had excellent candidates interested in the position (usually young and hungry new grads).
The problem is that the nocturnists mostly lasted a few years before flaming out, so there was a perpetual demand that exceeded supply. Some groups also excluded nocturnists from a partnership track, or had a different level of profit-sharing for those docs - a sense of inequality that was usually offset by a higher hourly rate for night shifts. This is how they attracted and retained not just nocturnists, but fast and efficient ones.
Create A Market For Buying Out Of Nightshifts
Some groups allowed motivated individuals to pay other members of equivalent status a standardized sum to take their night shifts. This worked best in places that had either an "eat what you kill" model where revenue reflected actual patient billings, or alternately, where all shifts paid the same.
What do I mean by equivalent status? Equity members / partners could not pay non-equity members or non-partners extra to take their nights. (It is common practice in many groups to either assign non-equity members more nights or to make a higher night burden part of the sweat equity investment toward full equity status. The groups I spoke to did not engage in this practice.)
It's important to note that this paying a colleague to take one or more nights was done on a completely voluntary basis. If you offered, for example, $400 for someone to take your night, and you had no takers, you either worked your night or raised your offer.
This is not the same as paying more for nightshifts and less for days. Recall from the initial post that in my group, we all take a comparable number of nights proportional to our target number of shifts. So someone who set their target shift load at 12 per month would be assigned twice the night shifts of someone with a target of 6 shifts per month on average.
Here is how it functions: Doc A is assigned an average of X night shifts in a typical month. Doc B is looking to increase income without increasing the total number of shifts he works. Many groups make their schedules via third party computer algorithms (our group uses shiftadmin) which allow you to customize how many nights and weekends each doc is assigned.
Since no month provides an exact number of nights, but the algorithm makes things even out in the long run, Doc B is assigned a target of one more nightshift per month and one fewer day shift. Doc A's targets are commensurately adjusted to one fewer night shift and more day per month.
After studying the various tactics, this was the option that ultimately made the most sense for me.
Before proceeding, I checked with the business manager who did the scheduling for our group. Was this an easy ask or a hard one? Fortunately, it turned out to be logistically easy for him, which meant implementation would not be an obstacle.
I Got My Group On Board
I called each equity member of my group to listen to their concerns and ask what it would take to craft a proposal that would garner their support. This part of the process was invaluable.
One colleague told me outright that if I didn't want to work nights, I should not be an emergency physician. Another suggested that buying out of nights was acceptable, but it would be a third rail if I suggested buying out of weekend shifts. Most folks were skeptical but open to the idea depending on how it was executed - responding along the lines of, "That's not something I want to utilize today, but it might be a nice option to have available in the future."
The unease was partly over the perception that buying out of nights was somehow a rich person's luxury that less well off docs could not afford. Was I creating a system of haves and have nots in what we currently considered to be a group of equals?
I had to do a bit of work explaining that, no, I was not a trust fund baby, I was simply willing to earn less income to pay for the privilege of working fewer nights - a privilege that each and every one of them would also have available. I was willing to pay for this the way other group members might choose private school, or a nice car, or a bigger house. No difference.
Did some of them still feel uncomfortable? Yes. Then we'd run into each other in the doctor's parking lot, and they'd see me getting out of my 2009 Kia Rondo, and they felt less suspicious of my financial position.
A final note: I had been an equity member for about a decade, and was a known and (hopefully) trusted member of my group at the time I made this attempt. I might not have tried to push an initiative like this as a newbie.
I Found Colleagues Willing To Work My Nights
After canvassing my group and feeling confident that I had the support to move forward, we formally voted to allow folks to buy out of nights.
Next, I had to figure out what the market rate was for buying out of a night shift our area. I called the few local ER directors who allowed buying out of nights and whose shop was run most similar to our own (independently run group, democratic, all hires have an explicit path to equity status) and confirmed that the going rate was $X.
I shared my findings with our group, and suggested that we establish a rate of $ X + 100, so that ours would be the best paying rate in the area. Everyone agreed. Setting a higher rate was advantageous in two ways: there was very little demand to begin (me, with one other person potentially interested but only after seeing how it went for me) and very little resentment (we were treating our people well with the highest rate in town).
Finally, I surveyed our group to see which equity members were interested in taking my nights. I found a match between supply and demand. I paid them as W2 employees, I automated their check payments so the check always came a couple of days early, and I checked in frequently to make sure they felt okay with the arrangement before and after it began.
It was the best money I ever spent, and I hope it was the easiest money they ever made.
I hope this explanation of the process of developing a playbook helps others who are looking to reduce their nightshift burden find a strategy that is deemed equitable by their groups.
In other news, I hope to resume posting once a week as part of a renewed effort to share updates, tackle subjects of interest, and continue to support you, fellow readers, as you figure out the most effective ways to become financially secure and reduce burnout. More on that in a future post
